Heart Health in Type 2 Diabetes: In the evolving landscape of diabetes management, heart health in type 2 diabetes has emerged as one of the most critical areas of research and clinical focus. Beyond blood sugar control, new findings suggest that some diabetes medications do more than manage glucose—they can actually protect the heart. A recent large-scale study has revealed that GLP-1 receptor agonists (GLP-1RAs), a class of glucose-lowering drugs, significantly reduce the risk of major cardiovascular events, positioning them as one of the most protective options available for patients with type 2 diabetes.
For decades, diabetes treatment revolved primarily around maintaining target blood sugar levels. While this approach effectively reduced complications like neuropathy and retinopathy, its effect on cardiovascular health remained uncertain. People with type 2 diabetes are two to four times more likely to experience heart attacks, strokes, or heart failure, making cardiovascular risk management a vital component of diabetes care. Now, the spotlight has shifted to medications that go beyond glycemic control, with researchers exploring which therapies best protect the heart while managing blood glucose.
The findings from a large comparative study involving nearly 300,000 adults with type 2 diabetes across six major U.S. health systems are helping reshape this conversation. The study compared four widely prescribed classes of diabetes drugs and revealed that GLP-1 receptor agonists delivered the strongest protection against major adverse cardiovascular events (MACEs), followed by SGLT2 inhibitors, sulfonylureas, and DPP4 inhibitors. These insights are redefining how clinicians approach treatment for patients at high cardiovascular risk.
Why Heart Health in Type 2 Diabetes Matters
A Dual Threat: High Blood Sugar and Heart Disease
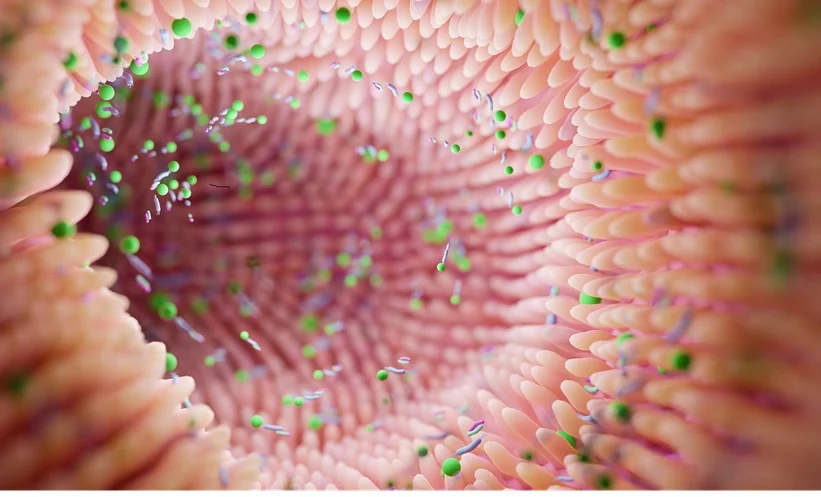
People with type 2 diabetes face a dual health challenge. Elevated blood glucose damages blood vessels over time, leading to atherosclerosis, or the buildup of plaque in arterial walls. This restricts blood flow and increases the risk of heart attacks and strokes. Moreover, insulin resistance, inflammation, and lipid imbalances common in diabetes further accelerate cardiovascular damage.
Studies estimate that more than 65% of people with diabetes die from heart disease or stroke. This staggering statistic underscores the need for therapies that target both metabolic and cardiovascular health simultaneously. Traditional medications like sulfonylureas and insulin focus primarily on glucose regulation but have shown mixed results in protecting the heart.
Cardiovascular Events: The Leading Cause of Mortality
Major adverse cardiovascular events (MACEs)—including heart attack, stroke, and cardiovascular death—remain the top causes of morbidity and mortality in type 2 diabetes patients. Because of this, the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) have both emphasized that treatment decisions should not only consider glucose control but also cardiovascular outcomes.
In recent years, this shift has prompted a growing body of research focused on cardioprotective diabetes medications, such as SGLT2 inhibitors and GLP-1 receptor agonists. These newer drug classes have been found to not only lower blood sugar but also improve heart and kidney health.
Comparative Study: Medications and Cardiovascular Outcomes
The Study Overview
In one of the largest comparative effectiveness studies of its kind, researchers evaluated data from 296,676 adults with type 2 diabetes across six major U.S. health systems. They compared four major medication classes:
- Sulfonylureas
- DPP4 inhibitors (DPP4is)
- SGLT2 inhibitors (SGLT2is)
- GLP-1 receptor agonists (GLP-1RAs)
A subset of 241,981 adults (mean age 57.2 years, 54.3% male) was further analyzed using advanced targeted learning methods to emulate a randomized trial. Over a 2.5-year follow-up, researchers tracked the incidence of major adverse cardiovascular events (MACEs) among patients using these medications.
The Findings
The study found that the 2.5-year risk of MACEs was lowest among those treated with GLP-1 receptor agonists, followed by SGLT2 inhibitors, sulfonylureas, and finally DPP4 inhibitors. Specifically:
- The cumulative risk difference was 1.9% higher for DPP4 inhibitors compared to sulfonylureas.
- The difference between SGLT2 inhibitors and GLP-1RAs was 1.5% (95% CI, 1.1%-1.9%), favoring GLP-1RAs.
Who Benefited the Most?
The cardiovascular benefits of GLP-1 receptor agonists were especially strong in:
- Patients aged 65 years or older
- Those with existing atherosclerotic cardiovascular disease (ASCVD)
- Patients with heart failure
- Individuals with mild to moderate kidney impairment
These results reinforce GLP-1RAs as a preferred therapy for patients at high risk of cardiovascular complications.
Read about: EACS 2025: Hepatitis B Reactivation Rare After Switching from Tenofovir, European Studies Show
Understanding GLP-1 Receptor Agonists
What Are GLP-1RAs?
GLP-1 receptor agonists are a class of injectable (and more recently, oral) medications that mimic the action of glucagon-like peptide-1 (GLP-1), a hormone naturally produced in the intestine. GLP-1 helps regulate blood sugar by:
- Stimulating insulin secretion after meals
- Suppressing excess glucagon release
- Slowing gastric emptying (which helps control appetite)
- Promoting a sense of fullness
Beyond these metabolic effects, research shows that GLP-1RAs improve endothelial function, reduce inflammation, and lower blood pressure—all of which contribute to cardiovascular protection.
Common GLP-1 Drugs
Commonly prescribed GLP-1RAs include:
- Liraglutide (Victoza)
- Semaglutide (Ozempic, Rybelsus)
- Dulaglutide (Trulicity)
- Exenatide (Bydureon, Byetta)
Many of these agents have demonstrated cardiovascular benefits in large-scale clinical trials, such as the LEADER and SUSTAIN-6 studies.

SGLT2 Inhibitors: The Strong Contender
While GLP-1RAs top the list for heart protection, SGLT2 inhibitors (like empagliflozin and dapagliflozin) also provide robust cardiovascular benefits. They work by promoting glucose excretion through urine, lowering blood sugar and reducing the workload on the heart. Moreover, SGLT2is are known to:
- Lower hospitalizations for heart failure
- Improve renal outcomes
- Reduce cardiovascular mortality
However, SGLT2 inhibitors are often considered more effective in younger patients or those without advanced ASCVD, whereas GLP-1RAs may be more beneficial for older adults or those with established heart disease.
Implications for Clinical Practice
The findings from this study provide valuable guidance for clinicians seeking to improve heart health in type 2 diabetes. With cardiovascular protection now recognized as a key treatment goal, GLP-1 receptor agonists should be strongly considered as first-line therapy—particularly for patients with high cardiovascular risk.
However, the study also highlights the need for individualized treatment plans. Clinicians must weigh factors such as:
- Cost and insurance coverage
- Accessibility and patient adherence
- Renal and hepatic function
- Potential side effects
As precision medicine continues to evolve, the future of diabetes care lies in tailoring therapy not just for glucose control but also for long-term cardiovascular safety.
The Future of Diabetes Care: Integrating Heart and Metabolic Health
The growing evidence supporting GLP-1 receptor agonists and SGLT2 inhibitors is transforming diabetes care from a glucose-centric to a cardiometabolic approach. These newer drug classes are not only improving life expectancy but also enhancing quality of life by reducing hospitalizations, complications, and healthcare costs.
Experts anticipate that within the next decade, treatment algorithms for diabetes will place cardiovascular protection at the forefront, with lifestyle modifications, early diagnosis, and pharmacogenomics all playing a role in personalized treatment strategies.
Conclusion
Heart health in type 2 diabetes is no longer a secondary consideration—it is now the central focus of modern diabetes care. The landmark study comparing different drug classes has brought clarity to a once-uncertain area of medicine, revealing that GLP-1 receptor agonists stand out as the most effective agents for reducing cardiovascular risk.
As more research validates these findings, doctors can confidently integrate GLP-1RAs into treatment plans for patients with existing heart disease or risk factors. Their dual benefit—controlling glucose and protecting the heart—makes them a cornerstone of comprehensive diabetes management.
The implications are far-reaching. By prioritizing heart health from the start, healthcare providers can reduce premature deaths, prevent complications, and improve the overall well-being of millions living with diabetes. While cost and accessibility remain barriers, the long-term savings from reduced hospitalizations and improved outcomes could make these therapies more widely available.
Ultimately, this shift marks a new era in diabetes care—one where cardiometabolic health takes precedence, and patients receive treatments that do more than lower blood sugar—they help them live longer, healthier lives.
Also read: Hyderabad Hospital Launches Genetic Test That Tells Which Medicines Work for You
Frequently Asked Questions
1. Why is heart health such a big concern for people with type 2 diabetes?
People with type 2 diabetes are at a higher risk of developing heart disease due to chronic high blood sugar, inflammation, and cholesterol imbalances. These factors damage blood vessels, leading to plaque buildup and increased risk of heart attacks or strokes. Managing heart health in diabetes is essential for reducing early mortality.
2. What makes GLP-1 receptor agonists beneficial for the heart?
GLP-1 receptor agonists mimic a natural hormone that regulates blood sugar, appetite, and metabolism. Beyond glucose control, they reduce blood pressure, inflammation, and oxidative stress—key contributors to cardiovascular disease. Clinical trials show they can significantly lower the risk of major adverse cardiovascular events.
3. How do GLP-1 receptor agonists compare with SGLT2 inhibitors for heart protection?
Both GLP-1RAs and SGLT2is offer heart-protective benefits but in different ways. GLP-1RAs reduce the risk of heart attack and stroke, while SGLT2is are more effective in preventing heart failure and improving kidney health. The choice depends on the patient’s age, medical history, and cardiovascular risk profile.
4. Are GLP-1 receptor agonists safe for everyone with type 2 diabetes?
Generally, GLP-1RAs are safe and well-tolerated, but they may cause mild side effects like nausea or vomiting initially. They’re not recommended for people with a history of certain thyroid cancers or severe gastrointestinal disease. Always consult a doctor before starting therapy.
5. What lifestyle changes complement GLP-1 therapy for better heart health?
Alongside medication, maintaining a balanced diet, regular physical activity, quitting smoking, managing stress, and controlling blood pressure and cholesterol are essential. Combining GLP-1 therapy with healthy lifestyle habits can dramatically improve both heart and metabolic health outcomes.