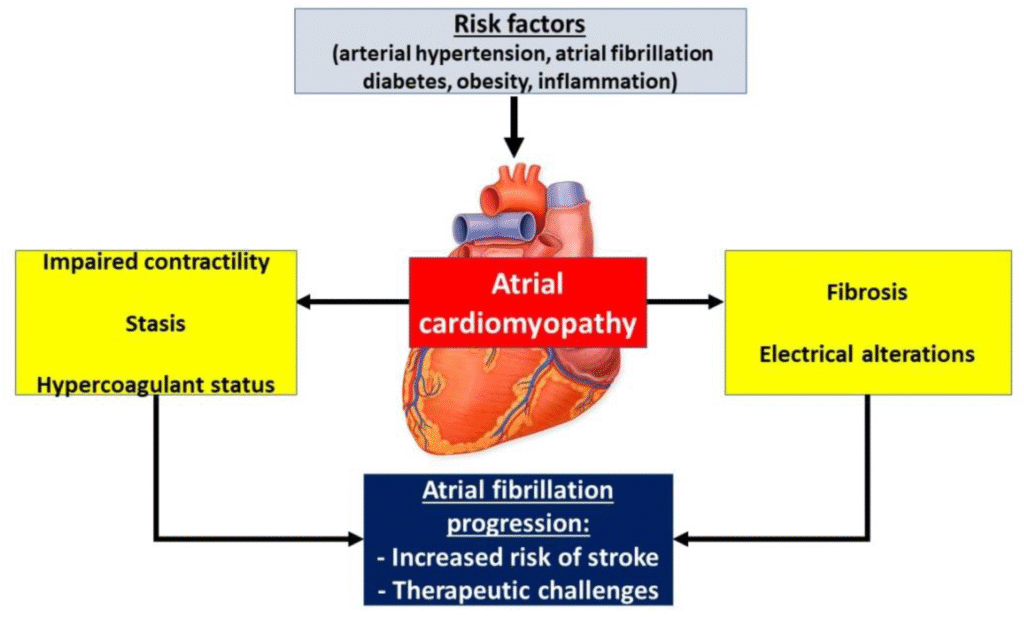
Atrial Cardiomyopathy Raises Stroke and Heart Risk: In a major advancement in cardiovascular research, a new UK Biobank study has revealed that atrial cardiomyopathy (AtCM) — a condition marked by electrical and structural abnormalities in the atria — is linked to significantly higher risks of atrial fibrillation (AF), stroke, and heart failure (HF). The findings emphasize that AtCM, once considered a secondary or incidental cardiac issue, may in fact represent a root cause of several major cardiovascular diseases.
For decades, doctors have understood that atrial fibrillation is a major risk factor for stroke. However, the exact mechanisms that predispose individuals to AF and subsequent cardiac events have remained unclear. This new large-scale analysis now positions atrial cardiomyopathy as a key driver of atrial remodeling — the electrical and structural changes that precede arrhythmia and heart dysfunction. The implications are profound, reshaping how cardiologists think about prevention, risk prediction, and treatment strategies for heart disease.
With over 26,000 participants analyzed, the study provides compelling evidence that identifying and managing AtCM early could help prevent severe outcomes like stroke and heart failure. Moreover, it reinforces the importance of controlling modifiable cardiovascular risk factors such as hypertension, diabetes, and coronary artery disease, which accelerate atrial changes.
Understanding Atrial Cardiomyopathy (AtCM)
What Is Atrial Cardiomyopathy?
Atrial cardiomyopathy refers to a group of structural, architectural, contractile, and electrical abnormalities affecting the atria — the upper chambers of the heart. Unlike traditional cardiomyopathies that primarily affect the ventricles, AtCM alters how the atria conduct electrical signals and manage blood flow, leading to impaired function and higher vulnerability to arrhythmias such as atrial fibrillation.
A Growing Focus in Cardiology
Historically, atrial changes were viewed as byproducts of atrial fibrillation or hypertension. But new research highlights that AtCM may actually precede and promote these conditions. It is now recognized as an early indicator of atrial disease progression, helping clinicians identify patients at higher risk for AF, stroke, and heart failure — even before symptoms appear.
Read about: Weight Gain Rates Stabilize After TNF Inhibitor Initiation in Psoriatic Arthritis
How Atrial Cardiomyopathy Predicts Major Cardiac Events
Findings from the UK Biobank Study
The UK Biobank study analyzed 26,467 individuals to explore the relationship between AtCM markers and cardiovascular outcomes. Researchers found that:
- 15.7% had at least one marker of AtCM.
- 2.3% had two or more markers, indicating more advanced disease.
Risk factors such as older age, hypertension, and coronary artery disease were strongly linked with AtCM presence. Importantly, the study quantified the increased risks:
- Those with one marker had a hazard ratio (HR) for atrial fibrillation of 1.88 (95% CI 1.54–2.31; P < .001).
- Those with two or more markers faced a dramatically higher HR of 4.59 (95% CI 3.52–5.99; P < .001).
The risk of heart failure increased by 3.08-fold (95% CI 2.03–4.66; P < .001), while the risk of stroke increased by 3.07-fold (95% CI 1.78–5.28; P < .001).
Furthermore, incorporating AtCM markers into risk prediction models improved the accuracy for AF diagnosis by a net reclassification improvement (NRI) of 13.7% (95% CI 9.2%–18.3%). This shows how identifying AtCM can refine clinical risk assessment.
Clinical Significance of Atrial Cardiomyopathy
The results suggest that AtCM may serve as a shared substrate for atrial fibrillation, stroke, and heart failure. In simple terms, the same structural and electrical atrial changes that lead to one condition can predispose patients to others. This interconnection highlights the importance of early detection, preventive management, and holistic cardiovascular care.
For clinicians, these findings underscore the need to incorporate AtCM markers into screening protocols for at-risk patients, especially those with long-standing hypertension, diabetes, or coronary artery disease. Early identification through imaging (such as cardiac MRI), ECG markers, or blood biomarkers may help predict who will develop AF or stroke before symptoms arise.
Risk Factors Associated with Atrial Cardiomyopathy
Some of the most notable risk factors for developing AtCM include:
- Advanced age
- Hypertension (high blood pressure)
- Coronary artery disease
- Obesity and metabolic syndrome
- Diabetes mellitus
- Excessive alcohol intake
- Sleep apnea
Addressing these risk factors through lifestyle modification, blood pressure control, and cholesterol management can significantly lower the risk of atrial remodeling and related cardiovascular events.
Future Outlook: Can AtCM Be Prevented or Reversed?
Ongoing research aims to determine whether early interventions can prevent or reverse atrial remodeling in patients with AtCM. One of the key ongoing trials, RACE X, is investigating whether catheter ablation — a procedure that targets the abnormal electrical pathways in the heart — can halt or even reverse atrial disease progression.
While no treatment currently exists to reverse AtCM entirely, controlling its root causes, such as high blood pressure, coronary artery disease, and inflammation, can slow its progression. Advances in genetic testing, artificial intelligence-based cardiac imaging, and biomarker analysis may soon allow physicians to detect AtCM earlier and personalize therapy.
Conclusion
The UK Biobank study marks a major milestone in understanding the link between atrial cardiomyopathy and serious cardiovascular outcomes. Once regarded as a secondary finding, AtCM now stands at the center of cardiac disease pathways — connecting atrial fibrillation, stroke, and heart failure.
Early identification of AtCM provides an opportunity to intervene before irreversible damage occurs. With a clear link between structural atrial changes and cardiovascular events, cardiologists can better target prevention strategies and improve patient outcomes.
Crucially, the study demonstrates that the risk rises sharply when multiple AtCM markers are present. This finding opens the door for more precise risk stratification, allowing doctors to prioritize high-risk patients for intensive management.
As science continues to uncover the complexities of atrial remodeling, the message is clear: atrial cardiomyopathy is no longer an incidental diagnosis but a critical warning sign that must be detected, monitored, and managed proactively.
Also read: Apple M4 MacBook Air vs M5 MacBook Pro (2025): Which One Should You Buy?
FAQs About Atrial Cardiomyopathy and Heart Risk
1. What exactly is atrial cardiomyopathy (AtCM)?
Atrial cardiomyopathy refers to structural and electrical abnormalities in the atria that impair their ability to contract and conduct signals properly. Over time, these changes increase the risk of arrhythmias such as atrial fibrillation and complications like stroke or heart failure. Unlike traditional heart muscle diseases that affect the ventricles, AtCM primarily targets the atria — the heart’s “receiving chambers.”
2. How does AtCM lead to stroke or atrial fibrillation?
AtCM causes the atria to remodel, leading to fibrosis (scarring) and impaired electrical conduction. These changes promote atrial fibrillation, which results in inefficient blood flow and pooling of blood in the atria. When blood clots form and travel to the brain, they cause ischemic strokes. Thus, AtCM acts as the foundation upon which AF and stroke develop.
3. Who is most at risk for developing atrial cardiomyopathy?
Older adults and individuals with hypertension, diabetes, coronary artery disease, obesity, or sleep apnea are most susceptible. Lifestyle factors such as excessive alcohol use, poor diet, and lack of exercise further contribute. Because the condition often develops silently, routine cardiac check-ups are vital for early detection.
4. Can atrial cardiomyopathy be reversed or cured?
Currently, there is no definitive cure for AtCM. However, its progression can be slowed — and in some cases partially reversed — through lifestyle modification and medical treatment. Controlling blood pressure, managing heart disease, reducing alcohol intake, and treating atrial fibrillation promptly can all help preserve atrial function.
5. What are the next steps in research and treatment?
Future studies like the RACE X trial aim to determine whether procedures such as catheter ablation can stop or reverse AtCM. Additionally, researchers are exploring advanced imaging techniques, biomarkers, and AI-based screening tools for earlier detection. These developments could enable personalized therapies that address the disease before it leads to AF or stroke.