Alcohol Raises Dementia Risk: For decades, the effects of alcohol on brain health have been hotly debated. While some studies suggested that light to moderate drinking might protect cognitive function, recent research tells a very different story. A new genetic study published in BMJ Evidence-Based Medicine demonstrates that alcohol consumption at any level — from light to heavy — can increase the risk of all-cause dementia. Using large observational cohorts and advanced genetic analyses, researchers confirmed that even moderate drinking may not be neuroprotective, challenging common beliefs about “safe” alcohol intake.
Dementia is a set of conditions that gradually impair memory, mood, decision-making, and daily functioning. It affects millions worldwide, and every three seconds, another family confronts its devastating consequences. As populations age globally, understanding modifiable risk factors like alcohol consumption is crucial. This study not only examines the relationship between drinking habits and dementia risk but also uses Mendelian randomization to distinguish correlation from causation — providing stronger evidence for lifestyle guidance, clinical counseling, and public health policies.
The implications are profound: alcohol, long considered by some to have potential cognitive benefits, now emerges as a clear contributor to dementia risk across all levels of consumption. Families, individuals, and healthcare professionals must reconsider drinking habits, especially when planning for long-term brain health.
Study Overview: How Alcohol and Dementia Are Linked
Researchers analyzed two large population cohorts: the Million Veteran Program (MVP) in the U.S. and the United Kingdom Biobank (UKB). They studied over 550,000 adults aged approximately 56–72 years, using electronic health records to track dementia diagnoses. Alcohol intake was measured both by drinks per week (DPW) and Alcohol Use Disorder (AUD) assessments.
The study incorporated:
- Observational analyses to evaluate real-world drinking patterns
- Longitudinal data to account for changes in alcohol consumption over time
- Genetic approaches using Mendelian randomization to separate causation from correlation
This comprehensive design allowed researchers to address biases often found in alcohol-dementia studies, including reverse causation (people reduce drinking as cognition declines) and confounding factors like education, income, and smoking.
Findings: Alcohol Increases Dementia Risk
Observational Analyses
Initial observational results suggested a U-shaped relationship: light drinkers seemed to have slightly lower dementia risk compared with non-drinkers or heavy drinkers. Heavy drinking (>40 DPW) and AUD were clearly associated with higher risk. However, longitudinal analyses revealed that this apparent protection for light drinkers was misleading — individuals who developed dementia tended to reduce alcohol consumption as symptoms emerged, explaining the U-shaped curve.
Read about: THIS Sweetest Fruit Can Keep Diabetes at Bay, New Study Finds
Genetic Evidence
Mendelian randomization (MR), which leverages genetic predispositions to higher alcohol intake, provided stronger evidence:
- Risk rises steadily with increasing alcohol consumption
- A one standard-deviation increase in genetically predicted alcohol intake was linked to a 15% higher odds of dementia
- A twofold increase in AUD prevalence corresponded to 16% higher odds of developing dementia
Importantly, MR analyses showed no protective effect at low levels of drinking, overturning the notion that moderate alcohol intake may benefit brain health.
Consistency Across Populations
While European-ancestry samples showed the strongest associations, African and Latin American ancestry groups also displayed increased dementia risk with AUD. The genetic evidence held after adjusting for age, sex, and other confounders.
Implications for Public Health and Daily Life
This study reinforces that no level of alcohol is completely safe for the brain. The findings have several practical implications:
- For Individuals and Families: Even moderate drinking can increase dementia risk. Limiting or abstaining from alcohol is advisable for long-term cognitive health.
- For Clinicians: Routine assessment of alcohol consumption should be part of cognitive health evaluations. Patients with a genetic predisposition or family history of dementia should be counseled on the risks of alcohol.
- For Policymakers: Reducing AUD prevalence could substantially lower the future burden of dementia. Estimates suggest that halving AUD prevalence may cut dementia cases by up to 16%.
The study underscores the importance of clear, consistent public messaging on alcohol and brain health — emphasizing risk at all levels, rather than implying a “safe” moderate threshold.
How to Protect Your Brain
- Limit or avoid alcohol consumption entirely if possible
- Adopt a brain-healthy lifestyle: regular physical activity, balanced diet, mental exercises, and social engagement
- Monitor cognitive health: routine checkups and early screenings for memory and cognitive function
- Manage other risk factors: control hypertension, diabetes, and cholesterol to reduce overall dementia risk
Conclusion
This genetic study fundamentally challenges the long-held belief that light to moderate alcohol consumption is protective for the brain. Evidence now shows a monotonic, dose-dependent increase in dementia risk with alcohol, highlighting that even moderate drinkers are not immune.
For individuals, families, and healthcare providers, these findings necessitate a reassessment of daily drinking habits. The study also emphasizes the importance of early prevention strategies — reducing alcohol use disorders could meaningfully lower dementia prevalence in the population.
Public health messaging must evolve to clearly communicate that no level of alcohol consumption is risk-free for cognitive health. By combining lifestyle interventions, early screening, and awareness, society can work toward reducing the future burden of dementia.
Also read: NCB Recruitment 2025: 37 डिप्टी डायरेक्टर और पब्लिक प्रॉसिक्यूटर पदों के लिए आवेदन करें
Frequently Asked Questions
1. Can light or moderate drinking protect the brain?
No. Genetic evidence from Mendelian randomization indicates that dementia risk rises steadily with alcohol consumption. Observed “protective” effects of light drinking in past studies are likely due to reverse causation and confounding.
2. What is alcohol use disorder (AUD), and how does it affect dementia risk?
AUD is a medical condition characterized by an inability to control alcohol consumption despite negative consequences. The study found that individuals with AUD have a significantly higher risk of developing dementia — up to 16% higher compared with non-AUD individuals.
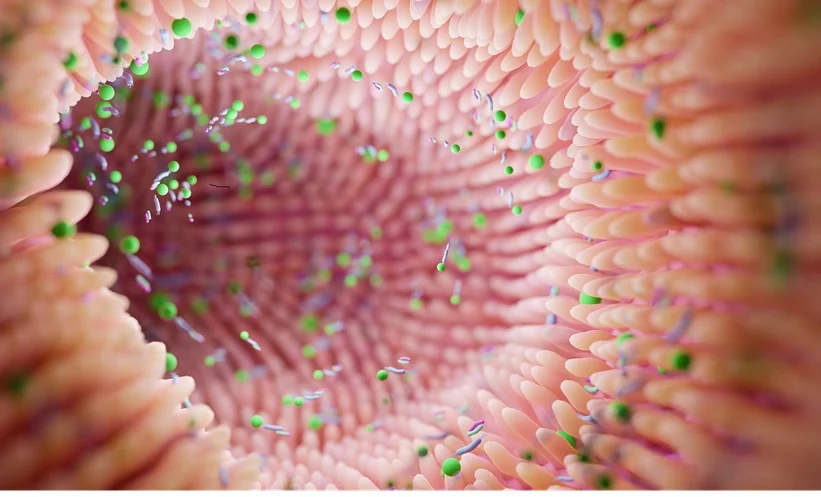
3. How does alcohol biologically contribute to dementia?
Alcohol can damage neurons, increase oxidative stress, and trigger inflammation in the brain. Over time, this impairs memory, cognition, and the brain’s ability to repair itself, contributing to all-cause dementia.
4. Does genetics influence the impact of alcohol on dementia risk?
Yes. The study used genetic variants to predict lifetime alcohol exposure and found a causal link to dementia. This suggests that both behavior and genetic predisposition interact to influence brain health outcomes.
5. What steps can I take to reduce my dementia risk related to alcohol?
Avoiding or minimizing alcohol consumption is the most effective strategy. Maintaining a brain-healthy lifestyle — including regular exercise, proper nutrition, stress management, and mental stimulation — also helps lower overall dementia risk.