COVID Brain Fog: The lingering effects of COVID-19 have continued to perplex scientists and medical professionals worldwide, even more than four years after the initial outbreak. While the acute phase of SARS-CoV-2 infection is well-documented, attention has increasingly shifted to the chronic condition known as Long COVID. Affecting millions globally, Long COVID presents with a constellation of persistent symptoms, ranging from fatigue and respiratory issues to cognitive impairments, often collectively referred to as “brain fog.” For many patients, this cognitive dysfunction severely disrupts daily life, making it difficult to focus, remember important details, or perform routine tasks efficiently. The scale of this problem has turned Long COVID brain fog into a significant public health challenge and socioeconomic concern, emphasizing the urgent need for research into its underlying biological mechanisms.
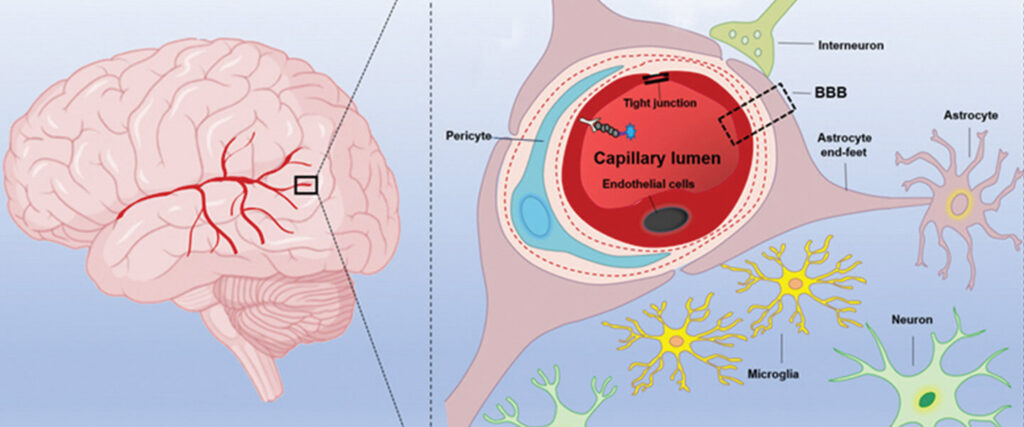
Despite widespread recognition of Long COVID, the precise causes of its cognitive symptoms have remained elusive. Previous neuroimaging studies revealed structural changes in the brains of some patients, but these findings fell short of explaining the molecular and functional disruptions that lead to brain fog. Scientists have struggled to identify objective biomarkers that could confirm Long COVID diagnosis or guide treatment strategies. The primary challenge lies in the difficulty of studying molecules that regulate communication between neurons, making it hard to pinpoint specific mechanisms behind cognitive impairment. Without such biomarkers, diagnosing and developing effective therapies for brain fog has remained largely speculative, limiting patient care and scientific understanding.
A groundbreaking study by researchers at Yokohama City University in Japan has now provided critical insights into the biological basis of Long COVID brain fog. Led by Professor Takuya Takahashi, the team employed an innovative brain imaging technique to directly observe changes in key neurotransmitter receptors associated with memory and learning. This research represents one of the most promising steps toward not only understanding the origins of Long COVID cognitive symptoms but also developing diagnostic tools and therapeutic strategies that could alleviate the condition for millions of sufferers worldwide.
Understanding Long COVID Brain Fog
What is Long COVID?
Long COVID is a chronic condition that can persist for weeks or months after the initial COVID-19 infection. Patients may experience a variety of symptoms, including fatigue, shortness of breath, sleep disturbances, and neurological issues. Among these, cognitive dysfunction—or brain fog—is one of the most debilitating, affecting over 80% of individuals diagnosed with Long COVID.
Symptoms and Impact
Patients often report difficulties with memory, concentration, and problem-solving. These cognitive impairments can affect professional performance, social interactions, and overall quality of life. The widespread prevalence of these symptoms underscores the urgent need for objective measures to understand and treat Long COVID brain fog effectively.
Read about: Silent Heart Attacks: Symptoms That Whisper, Not Shout
The Breakthrough in Brain Imaging
The Role of AMPA Receptors
Prior research in psychiatric and neurological disorders such as depression, bipolar disorder, schizophrenia, and dementia highlighted the importance of AMPA receptors (AMPARs) in memory and learning. Professor Takahashi’s team hypothesized that similar disruptions in AMPAR expression might underlie cognitive symptoms in Long COVID patients.
Using [11C]K-2 AMPAR PET Imaging
To test this hypothesis, the researchers utilized a novel imaging technique called [11C]K-2 AMPAR PET. This method allows scientists to visualize and quantify AMPAR density in the living human brain, providing direct insights into molecular changes associated with cognitive dysfunction.
Key Findings
By analyzing 30 Long COVID patients and comparing their data to 80 healthy controls, the team observed a widespread increase in AMPAR density across multiple brain regions. Importantly, higher AMPAR levels were directly correlated with the severity of cognitive symptoms. Additionally, inflammatory markers were found to interact with receptor expression, suggesting a link between systemic inflammation and brain receptor changes.
Implications for Diagnosis and Treatment
Diagnostic Potential
The study demonstrated that AMPAR PET imaging could distinguish Long COVID patients from healthy individuals with 100% sensitivity and 91% specificity. This finding suggests that imaging could serve as a reliable biomarker for diagnosing Long COVID brain fog, offering a much-needed objective tool for clinicians.
Therapeutic Strategies
The identification of elevated AMPARs also opens new avenues for treatment. Drugs that modulate AMPAR activity could potentially alleviate cognitive symptoms in patients suffering from Long COVID. This discovery marks an important step toward developing targeted therapies for a condition that has long lacked effective medical interventions.
Conclusion
The recent findings from Professor Takahashi and his team provide a concrete biological explanation for Long COVID brain fog, addressing a major gap in current medical knowledge. By linking elevated AMPA receptor density to cognitive symptoms, the study offers both a diagnostic biomarker and a potential therapeutic target, paving the way for innovative approaches to treatment.
This breakthrough also validates the experiences of millions of Long COVID patients who have struggled with cognitive impairments for years. Recognizing brain fog as a legitimate clinical condition could accelerate research efforts and increase healthcare support for affected individuals.
Moreover, the integration of advanced imaging techniques like [11C]K-2 AMPAR PET into clinical practice could transform how neurological symptoms of Long COVID are identified and monitored. Early and accurate diagnosis may lead to more personalized interventions, improving patient outcomes and reducing the long-term socioeconomic burden of the condition.
Finally, these findings highlight the importance of continued research into the neurological effects of SARS-CoV-2. While further studies are needed to develop definitive treatments, this study represents a promising milestone in understanding and managing Long COVID brain fog, offering hope to millions worldwide.
Also read: Recurrent UTIs: Why Some Women Keep Getting Them
Frequently Asked Questions
1. What causes brain fog in Long COVID patients?
Brain fog in Long COVID is linked to disruptions in neuronal communication, specifically involving AMPA receptors (AMPARs) in the brain. Elevated AMPAR density, as revealed through PET imaging, has been shown to correlate with cognitive symptoms such as memory loss, difficulty concentrating, and mental fatigue. Systemic inflammation may further influence receptor expression, exacerbating the condition.
2. How common is brain fog among Long COVID patients?
Research suggests that over 80% of Long COVID patients experience some degree of cognitive impairment. Brain fog can range from mild concentration difficulties to severe memory lapses and executive dysfunction, significantly impacting daily life and professional performance.
3. What is [11C]K-2 AMPAR PET imaging?
[11C]K-2 AMPAR PET imaging is a specialized brain imaging technique that allows researchers to visualize and quantify the density of AMPA receptors in the living brain. This technology helps identify molecular changes associated with cognitive symptoms and provides an objective biomarker for diagnosis and treatment planning.
4. Are there treatments available for Long COVID brain fog?
Currently, no specific treatments target Long COVID brain fog. However, the discovery of elevated AMPARs opens the possibility of using drugs that modulate these receptors to alleviate symptoms. Ongoing research aims to develop therapies based on these molecular insights.
5. Can brain fog from Long COVID be fully reversed?
Recovery varies among patients. While some individuals experience gradual improvement over time, others may continue to face persistent cognitive difficulties. Advances in diagnostic imaging and potential therapies targeting AMPARs may enhance recovery prospects in the future.