Rising Global Childhood CKD Highlights Health Inequality Gaps: Chronic kidney disease (CKD) among children and adolescents is emerging as a significant — and deeply unequal — global health challenge. A new analysis based on data from the Global Burden of Disease Study 2021 provides one of the most comprehensive evaluations to date of CKD trends in individuals aged 0–19 years. The findings reveal not only the scale of the problem but also widening disparities tied closely to socioeconomic development, healthcare access, and regional infrastructure.
A Growing Global Burden
According to the study, an estimated 7.54 million children and adolescents worldwide were newly affected by CKD in 2021, corresponding to an age-standardised incidence rate (ASIR) of 28.62 per 100,000 population. These figures highlight that CKD is far from rare in younger populations, challenging the long-standing perception that kidney disease is primarily an adult health issue.
The data show marked regional variation. Central Asia recorded the highest incidence rates, while regions classified under the low-middle Socio-Demographic Index (SDI) experienced the fastest growth in new cases over time. The SDI is a composite measure reflecting income per capita, educational attainment, and fertility rates, commonly used to assess developmental progress across countries.
While some high-income regions have seen stabilisation or modest declines in incidence, many lower-SDI areas continue to experience steady increases, underscoring systemic health inequities.
Adolescents at Increasing Risk
One of the most striking findings of the analysis is the sharp rise in CKD incidence among adolescents aged 14–19 years. This age group experienced an increase of more than 44% over the study period. Several factors may contribute to this trend, including improved diagnostic recognition, rising rates of hypertension and diabetes in youth, congenital kidney anomalies progressing with age, and environmental exposures.
Adolescence is a critical developmental window. CKD during this period can have long-term consequences, including delayed growth, cardiovascular complications, reduced quality of life, and increased risk of progression to end-stage kidney disease in early adulthood.
The rising adolescent burden also highlights the need for targeted screening strategies in schools and community health settings.
Mortality and Disability: Inequality in Outcomes
Beyond incidence, the study evaluated mortality rates and disability-adjusted life years (DALYs), a measure that combines years of life lost due to premature death with years lived with disability.
Mortality rates were strongly correlated with socioeconomic development. Lower-SDI regions experienced significantly higher CKD-related death rates compared to higher-income regions. This gap reflects disparities in early diagnosis, availability of specialist care, access to medications, and infrastructure for kidney replacement therapy.
Investigators observed that the concentration index for CKD-related DALYs became more negative between 1990 and 2021. In practical terms, this means the disease burden is increasingly concentrated among disadvantaged populations.
Children born in lower-income regions are more likely to:
- Be diagnosed later in the disease course
- Lack consistent access to nephrology services
- Face barriers to dialysis or transplantation
- Experience preventable complications
The inequality is not only geographic but structural.
Also read: Muthoot Finance MD Explains Flat Gold Tonnage, Loan Growth Outlook as Stock Slides
The Role of Kidney Replacement Therapy (KRT)
Access to kidney replacement therapy — including dialysis and kidney transplantation — emerged as a decisive factor in determining outcomes.
Regions with greater availability of KRT consistently demonstrated lower CKD-related disability burdens. Conversely, limited access often translates into preventable mortality and prolonged suffering.
In many low-resource settings:
- Dialysis centres are scarce
- Treatment costs are prohibitive
- Pediatric transplant programmes are limited
- Travel distances create logistical barriers
Children requiring long-term dialysis may face interrupted education, financial strain on families, and psychosocial stress. Where transplantation is unavailable or delayed, mortality risk rises substantially.
The study underscores that equitable investment in KRT infrastructure is essential for narrowing survival gaps.
Long-Term Projections to 2050
Using a Bayesian Age-Period-Cohort modelling approach, researchers projected that global incidence rates may gradually decline by 2050. The ASIR is expected to fall to approximately 25.54 per 100,000 population.
However, the authors caution that improvements are unlikely to be evenly distributed without deliberate policy action. Historical patterns suggest that high-SDI regions will benefit first from advances in early detection and treatment, potentially widening disparities further if lower-income regions are left behind.
Declines in incidence may also reflect improved maternal health, better management of congenital anomalies, and stronger public health surveillance — but only where healthcare systems are robust.
Importance of Early Detection
A recurring theme in the analysis is the need for earlier detection strategies, particularly in low- and middle-income countries.
Early CKD is often asymptomatic. Without screening programmes, diagnosis may occur only after significant kidney damage has occurred.
Strengthening early detection could involve:
- Routine urine testing in school health programmes
- Screening high-risk children with family histories of kidney disease
- Monitoring children with congenital urinary tract anomalies
- Improving primary care awareness
Timely intervention can slow disease progression, reduce cardiovascular complications, and improve long-term survival.
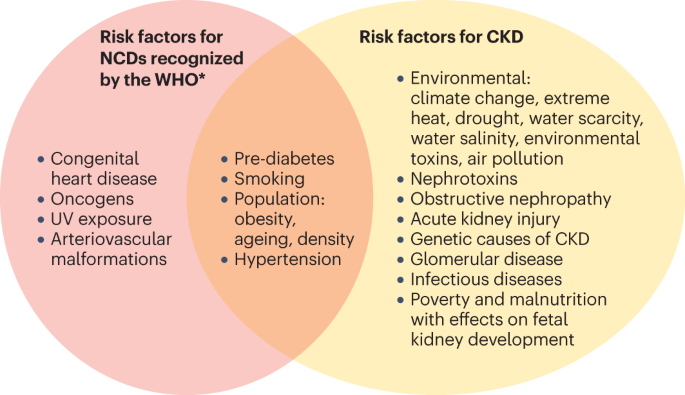
Socioeconomic Drivers of Risk
The study also highlights broader determinants of paediatric CKD risk, including:
- Poor prenatal and maternal health
- Limited access to clean water and sanitation
- Exposure to environmental toxins
- Malnutrition
- Limited education and health literacy
Socioeconomic disadvantage compounds biological vulnerability. Children in resource-poor settings may face cumulative risks that increase susceptibility to kidney damage and limit recovery.
Addressing CKD, therefore, requires not only medical solutions but social policy interventions.
Policy Implications
The findings call for coordinated global action. Key priorities include:
- Expanding paediatric nephrology training and workforce capacity
- Increasing investment in dialysis and transplant infrastructure
- Integrating CKD screening into national child health programmes
- Strengthening universal health coverage to reduce financial barriers
- Supporting public education on kidney health
International partnerships and targeted funding mechanisms may be essential to ensure equitable progress.
Read about: Olympic Games Athletes Push Their Bodies to the Limit. Should We?
A Call to Close the Gap
While the projected global decline in CKD incidence offers cautious optimism, the current trajectory reveals a troubling pattern: the burden of disease is increasingly concentrated among those with the least access to care.
Paediatric CKD is not merely a clinical issue. It is a reflection of global inequality.
The study reinforces that meaningful progress will depend on reducing socioeconomic disparities, investing in early detection, and ensuring that life-saving treatments are accessible to all children — regardless of where they are born.
Without deliberate and inclusive policy measures, the world risks perpetuating a cycle in which vulnerable populations continue to bear the heaviest burden of chronic kidney disease well into the future.