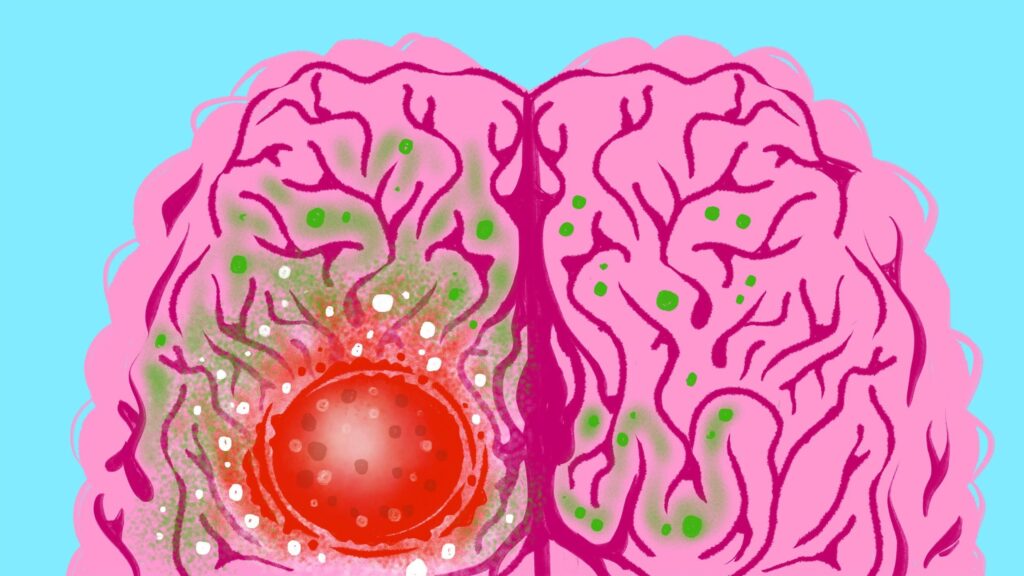
Starving Cancer: Glioblastoma is one of the most aggressive forms of malignant brain tumors, and survival rates remain alarmingly low, typically just one to two years after diagnosis. Traditional treatments—surgery, radiation, and chemotherapy—offer only temporary relief, as these tumors often return and develop resistance. However, recent research at the University of Michigan offers a new glimmer of hope. By targeting the unique ways brain cancer cells process nutrients, scientists have discovered that a specialized diet can significantly slow tumor growth in mice, potentially paving the way for new treatment approaches for patients.
Unlike healthy brain cells, glioblastoma cells rewire their metabolism to prioritize growth and invasion over normal brain function. Ordinary brain tissue uses sugar primarily for energy and neurotransmitter production, which is essential for cognitive processes and overall brain health. Glioblastoma cells, however, divert these nutrients into the production of molecules that fuel cancer proliferation, essentially “hijacking” the brain’s resources. Understanding this metabolic difference has opened a promising avenue for dietary interventions to slow tumor progression.
The University of Michigan team, including researchers from the Rogel Cancer Center, Department of Neurosurgery, and Department of Biomedical Engineering, conducted extensive studies in both mice and patients. By tracing labeled sugars injected into subjects, they discovered a “metabolic fork in the road” that differentiates healthy brain tissue from cancerous tumors. Their findings provide crucial insights into potential strategies that combine diet, chemotherapy, and radiation to improve patient outcomes.
How Brain Cancer Cells Exploit Sugar Metabolism
Metabolic Differences Between Healthy Brain Cells and Glioblastomas
Metabolism allows cells to break down nutrients such as carbohydrates and proteins to generate energy or build essential molecules. While both normal brain cells and glioblastomas require sugar, they use it very differently:
- Healthy Brain Cells: Convert sugar into energy and neurotransmitters necessary for brain function.
- Glioblastomas: Redirect sugar to produce nucleotides, the building blocks of DNA and RNA, supporting rapid cell growth and tumor invasion.
This metabolic rerouting also extends to amino acids. Healthy brain tissue synthesizes amino acids from sugar, whereas glioblastomas rely on scavenging these molecules directly from the bloodstream, creating a new vulnerability that researchers can exploit.
Targeting Amino Acid Pathways: A Novel Dietary Approach
Serine and Glycine Restriction
The research team hypothesized that limiting certain amino acids in the diet could selectively affect tumor cells while sparing normal brain function. They tested this theory in mice, restricting the amino acids serine and glycine, which are crucial for tumor growth.
- Mice fed an amino acid-restricted diet showed smaller tumors.
- Tumors responded better to radiation and chemotherapy compared to mice fed normal diets.
This approach takes advantage of the tumor’s reliance on blood-borne amino acids, likening the cancerous pathway to a busy freeway, while normal brain uptake resembles a slower country road. By “blocking the freeway,” researchers can potentially starve the tumor without harming healthy tissue.
Mathematical Modeling of Metabolic Pathways
To further optimize treatment strategies, the team developed mathematical models that map glucose usage across different metabolic pathways. These models can help identify other “roadblocks” where drugs or dietary interventions could selectively target cancer cells, offering a personalized and precise approach to treatment.
Implications for Human Patients and Future Clinical Trials
The promising results in mice have set the stage for clinical trials aimed at testing specialized amino acid-restricted diets in glioblastoma patients. While the therapy is still experimental, the multidisciplinary collaboration at the University of Michigan is bringing together oncology, neurosurgery, and biomedical engineering expertise to translate these findings from the lab to the clinic.
“By understanding and exploiting the metabolic vulnerabilities of glioblastomas, we hope to create new treatment opportunities that improve patient outcomes,” said Daniel Wahl, M.D., Ph.D., co-senior author of the study.
Conclusion
Glioblastomas remain one of the deadliest forms of brain cancer, largely due to their aggressive growth and resistance to conventional therapies. However, targeting the unique metabolic pathways of these tumors provides a promising new strategy.
By altering the availability of key nutrients such as serine and glycine, researchers have demonstrated in mice that tumor growth can be slowed, and treatment outcomes improved. This approach capitalizes on the tumor’s reliance on blood-derived nutrients while sparing normal brain tissue.
The University of Michigan study highlights the power of combining diet, metabolic research, and conventional therapies to create innovative treatment strategies. If successful in human trials, these findings could revolutionize the way glioblastoma is treated.
As clinical trials move forward, ongoing research will refine dietary strategies, explore additional metabolic targets, and provide hope for patients facing one of the most challenging cancers. With continued multidisciplinary collaboration, starving cancer may become a viable tool in the fight against glioblastoma.
Also read: New 2026 Mercedes GLA to Rival Volkswagen Golf, ID 3 with Electric and Hybrid Powertrains
Frequently Asked Questions
1. What is glioblastoma and why is it so deadly?
Glioblastoma is an aggressive type of brain cancer that grows rapidly and spreads into surrounding tissue. It is resistant to conventional treatments like surgery, chemotherapy, and radiation, resulting in a median survival of only one to two years after diagnosis.
2. How do glioblastoma cells metabolize sugar differently from normal brain cells?
While healthy brain cells convert sugar into energy and neurotransmitters, glioblastoma cells redirect sugar to produce nucleotides and other molecules that fuel rapid cell growth and tumor invasion. This metabolic reprogramming is a vulnerability that can be exploited through diet or targeted therapies.
3. What is the role of amino acids like serine and glycine in tumor growth?
Glioblastomas rely on amino acids from the blood to build proteins and DNA, unlike normal brain tissue, which can synthesize these amino acids internally. Limiting dietary serine and glycine can “starve” the tumor, slowing growth and enhancing treatment efficacy.
4. How did the University of Michigan researchers test this approach?
The team fed mice an amino acid-restricted diet and monitored tumor growth alongside chemotherapy and radiation. Tumors in mice on the restricted diet were smaller and more responsive to treatment, demonstrating the potential of dietary interventions.
5. Are there plans for clinical trials in humans?
Yes, researchers are preparing clinical trials to test amino acid-restricted diets in glioblastoma patients. The goal is to determine if the strategy that worked in mice can safely and effectively enhance treatment outcomes in humans.