EACS 2025: Hepatitis B reactivation has long been a concern for people living with HIV who switch antiretroviral therapy (ART) regimens. Tenofovir, available as tenofovir disoproxil fumarate (TDF) or tenofovir alafenamide (TAF), has proven effective not only in suppressing HIV but also in controlling hepatitis B virus (HBV). With the rising adoption of tenofovir-sparing ART regimens, such as dolutegravir/lamivudine and cabotegravir/rilpivirine, clinicians and patients have been cautious about the potential risk of HBV reactivation after discontinuing tenofovir.
At the 20th European AIDS Conference (EACS 2025) in Paris, two major European studies addressed this concern, providing reassuring data for physicians and patients. Both the Swiss HIV Cohort and the Hospital Clinic in Barcelona investigated HBV reactivation incidence in people switching from tenofovir-containing regimens to tenofovir-sparing ART. The results indicate that hepatitis B reactivation is extremely rare, even among patients with past exposure to HBV.
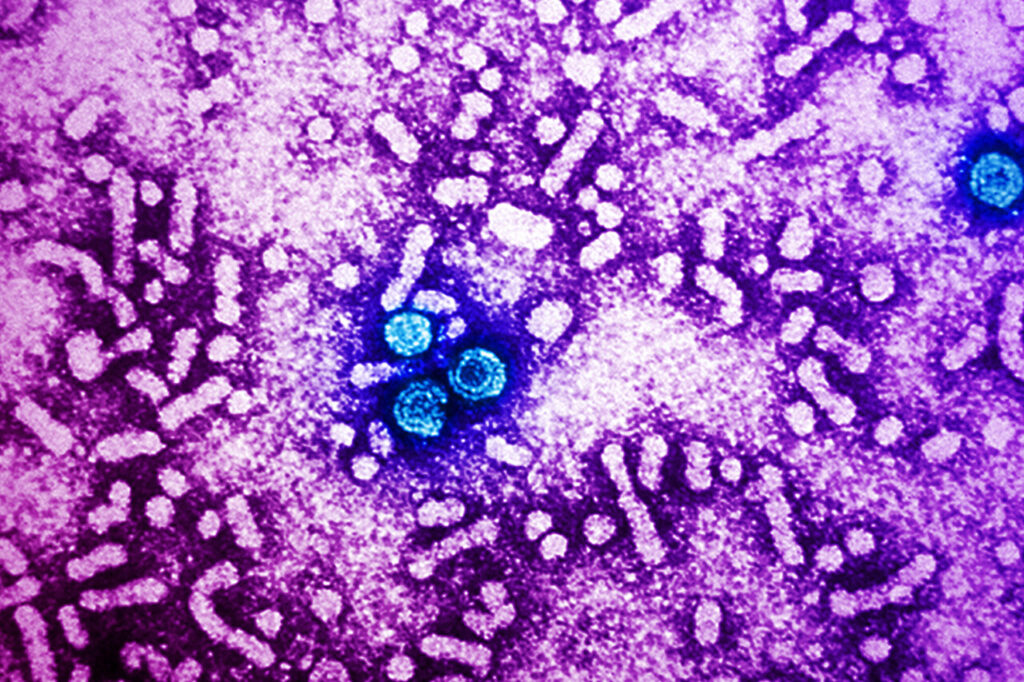
Understanding the nuances of HBV reactivation is crucial because of the virus’s persistence in the liver. Hepatitis B cccDNA, a stable viral form in hepatocyte nuclei, is not eliminated by antiviral therapy, meaning reactivation is possible if protective drugs are withdrawn. However, these studies highlight that, with proper monitoring and vaccination, switching to tenofovir-sparing regimens can be safe for most patients with HIV.
Hepatitis B Reactivation: What You Need to Know
Mechanism of Reactivation
HBV reactivation occurs when suppressed virus resumes replication, often triggered by the withdrawal of antiviral drugs, immunosuppression, aging, cancer, or loss of vaccine-induced immunity. It can lead to liver inflammation, cirrhosis, or hepatocellular carcinoma (HCC) if undetected. Past exposure to HBV is indicated by the presence of anti-HBc antibodies, whereas vaccination produces anti-HBs antibodies without anti-HBc.
Monitoring and Detection
Reactivation is often detected via elevated liver enzymes (ALT) and the presence of HBV DNA or hepatitis B surface antigen (HBsAg). Increases in liver enzymes should trigger further testing to ensure early identification of reactivation or acute infection.
Read about: CHEST 2025: New Algorithm Enhances AATD Diagnosis Accuracy
Study 1: Swiss HIV Cohort
The Swiss HIV Cohort examined 197 patients switching to tenofovir-sparing regimens without emtricitabine or lamivudine and compared them with 197 patients continuing regimens containing these HBV-active drugs. Key findings include:
- Anti-HBc positivity: Nearly one-third of participants.
- HBV DNA detection: Only 1.4% had detectable HBV DNA post-switch.
- ALT flares: No significant difference between groups; flares >80 IU/L were rare.
- Reactivation incidence: 5.6% in the non-HBV-active regimen group versus 1.1% in the HBV-active regimen group, but HBV DNA remained below quantifiable limits, and no HBsAg positivity was detected.
Dr. Lorin Begré concluded that switching to non-tenofovir regimens is generally safe for patients with HIV who have past HBV exposure.
Study 2: Hospital Clinic, Barcelona
The Barcelona study followed 741 participants switching to injectable cabotegravir/rilpivirine. Participants were monitored for liver enzyme elevations and HBV markers over a median follow-up of 54 weeks.
Key observations:
- Baseline HBV status: 0.5% chronic infection, 22% resolved infection, 3% isolated anti-HBc positivity, 61% vaccinated, 12% unprotected.
- Liver enzyme elevations: 17% of participants experienced elevations, but there was no significant difference between HBV exposure groups.
- Reactivation: No reactivation occurred, except in two participants with previously undetected chronic HBV. Both were successfully resuppressed after resuming tenofovir-containing therapy.
Professor Sanjay Bhagani emphasized that concerns about HBV reactivation in tenofovir-sparing switches may be overstated when proper monitoring is applied.
Implications for HIV Care
While the risk of HBV reactivation is extremely low, counseling and monitoring remain essential. Patients with anti-HBc antibodies or without HBV immunity should be considered for hepatitis B vaccination. Routine monitoring of liver enzymes, HBV DNA, and HBsAg ensures that rare reactivation events are promptly addressed. These studies provide reassurance that tenofovir-sparing regimens can be used safely in carefully selected patients.
Conclusion
The 2025 European AIDS Conference presented two large European studies confirming that hepatitis B reactivation is rare after switching from tenofovir-containing ART. Both the Swiss HIV Cohort and the Barcelona prospective study showed very low incidences of reactivation, even among patients with past HBV exposure.
For clinicians, these findings highlight the feasibility of using tenofovir-sparing two-drug regimens without significantly increasing HBV risk. This is especially relevant for patients seeking simplified or injectable HIV treatment options.
However, vigilance remains key. Regular liver enzyme monitoring and serological testing are recommended, particularly for patients who are anti-HBc positive or lack HBV immunity. Proper vaccination strategies further reduce the risk of acute hepatitis B infection.
Overall, the studies offer reassurance to HIV care providers and patients, emphasizing that with appropriate monitoring, tenofovir-sparing ART regimens are a safe alternative for the majority of patients.
Also read: Non-Alcoholic Fatty Liver Disease (NAFLD): What Really Causes It and How to Fix It
FAQs: Hepatitis B Reactivation in HIV Patients
1. What is hepatitis B reactivation?
Hepatitis B reactivation occurs when the virus resumes replication in a patient whose infection was previously suppressed. Reactivation can lead to liver inflammation, elevated ALT levels, cirrhosis, or hepatocellular carcinoma if not detected and treated promptly.
2. Who is at risk of HBV reactivation when switching ART?
Patients with HIV who have anti-HBc antibodies (indicating past HBV exposure) or those lacking HBV immunity are at risk. Immunosuppressed individuals and those with undetected chronic HBV are also vulnerable. Proper screening and monitoring are essential.
3. How common is HBV reactivation after switching from tenofovir?
According to the Swiss and Barcelona studies, HBV reactivation is very rare. The Swiss cohort reported 5.6% reactivation in non-HBV-active regimens, with undetectable HBV DNA and no HBsAg positivity, while the Barcelona study observed reactivation only in two participants with undetected chronic HBV.
4. How is HBV reactivation detected?
Reactivation is usually detected via elevated liver enzymes (ALT), HBV DNA quantification, and HBsAg testing. Any liver enzyme increase in anti-HBc positive patients should prompt further HBV testing to rule out reactivation.
5. Can tenofovir-sparing ART regimens be used safely?
Yes. Both studies indicate that with proper monitoring and vaccination, tenofovir-sparing regimens like dolutegravir/lamivudine or cabotegravir/rilpivirine are safe for patients with HIV, including those with past HBV exposure. Early detection of rare reactivation events allows timely intervention.











z1ya22